Author: Dr Hitesh Patel
The recorded sessions from the annual GP symposium, including sessions on heart failure, are available online to view. At the most recent symposium I reviewed treatment of heart failure. In this newsletter we focus on HFpEF. It is now often stated that of the new diagnosis of heart failure, half are those with preserved left ventricular ejection fraction. Patients with HFpEF are older than those with reduced ejection fraction and have the same mortality risk.
Diagnosis
Patients might present with overt congestive heart failure, with preserved ejection fraction, without valvular heart disease, and without other confounders such as severe anaemia, acute renal failure or thyrotoxicosis. Others, that might potentially have HFpEF, could present reporting problems with shortness of breath on exertion without overt congestion, and without significant coronary artery disease or other problems, such as lung disease.
Parameters measured with echocardiography
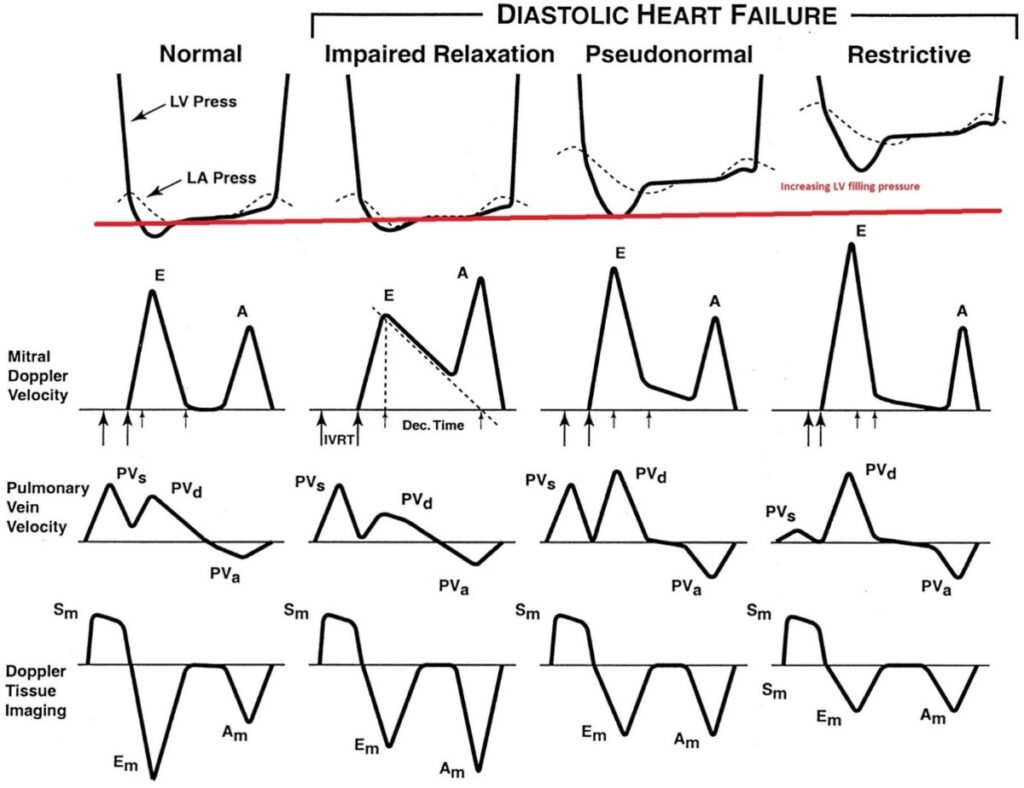
The graphic below from a review article in Circulation in the year 2002 illustrates the impact of increasing diastolic dysfunction on left ventricular filling pressures and on the flow velocity of blood across the mitral valve during diastole, and the impact on the velocity of mitral annulus in diastole.
E/A ratio
Early filling of the left ventricle occurs at the beginning of diastole and late in diastole there is additional filling from atrial contraction. The early filling peak velocity (E velocity) and peak velocity from atrial contraction (A velocity) can be measured, the E/A ratio is calculated.
In the earliest stage of diastolic dysfunction the E/A ratio decreases with E velocity less than A velocity (E/A less than 0.8). As dysfunction progresses and with increase of LV filling pressure (left atrial pressure has to also increase) the flow pattern across the mitral valve alters, the E/A ratio “normalises” and in advanced stages the E wave velocity is more than twice the A wave velocity (E/A ratio >2).
E/e’ ratio
As diastolic dysfunction worsens the mitral valve annular velocity in early diastole progressively decreases- the early annular velocity in diastole is referred to as the e’ velocity. The ratio of the E wave velocity and the annular e’ velocity (E/e’ ratio) increases with worsening diastolic dysfunction.
Left atrial volume
As we might expect, as the left atrial pressures rises to enable filling of the left ventricle with diastolic dysfunction, the left atrium will dilate. The degree of left atrial dilation can be viewed as a barometer of chronic elevation of pressures in the left atrium. When the left atrial volume (indexed to body surface area) is greater than 34 ml/m2 then this is consistent with presence of significant chronically elevated left atrial pressures, and when this is not due to other conditions including mitral valve regurgitation, hypertrophic cardiomyopathy or cardiac amyloidosis.
Elevated pulmonary artery systolic pressures
We can understand that as left atrial pressure rises with diastolic dysfunction, the pulmonary venous and pulmonary artery pressures will also be higher. When there is tricuspid valve regurgitation, even mild, the peak velocity of the tricuspid regurgitant jet can be measured, the peak tricuspid regurgitation jet velocity estimates the pulmonary artery pressure using a simple formula (4v2 plus estimated right atrial pressure). A velocity greater than 2.8m/s supports the diagnosis of HFpEF if not due to any other condition, including advanced lung disease.
BNP measurement
As is well known, the BNP level can be measured to rule out or rule in heart failure. Generally, a non-elevated BNP level rules out heart failure, However, it is stated that up to 20% of patients with invasively proven HFpEF have BNP levels below diagnostic thresholds, particularly in the presence of obesity. BNP levels are higher at any time in those with atrial fibrillation and renal failure.
Algorithms to assist with diagnosis of HFpEF
The 2021 European Cardiac Society heart failure guideline does include a caution regarding use of two algorithms that are discussed below, stating that diagnostic performance has varied. The two algorithms take a different approach and hence are not expected to always be concordant.
H2FPEF
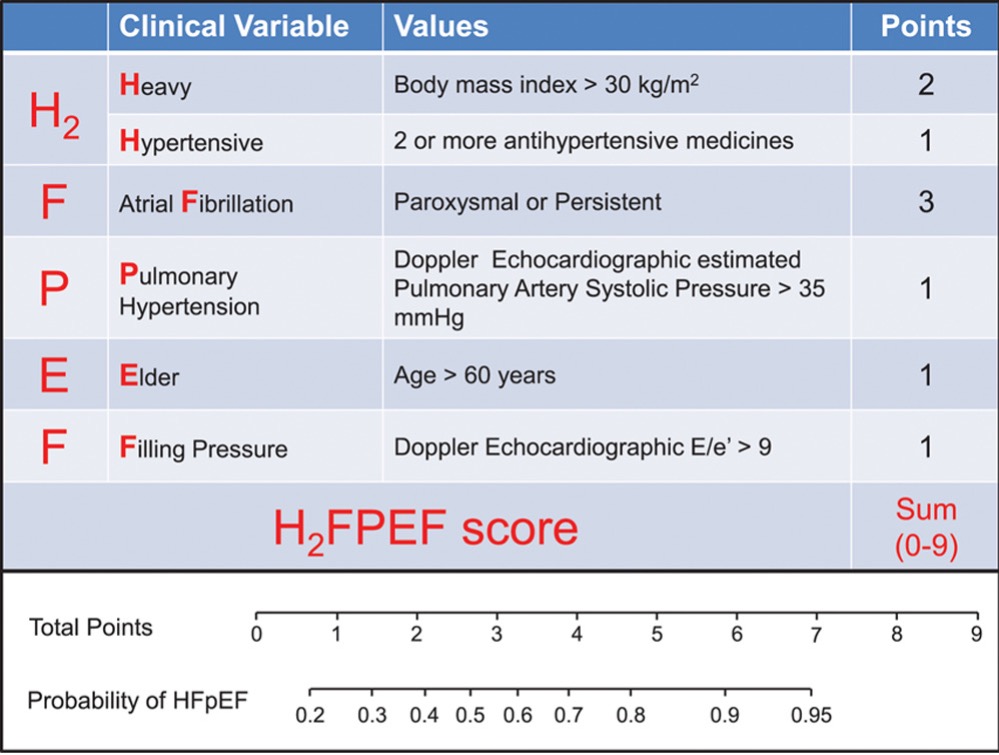
In this algorithm 4/6 variables are clinical variables. An obese individual with hypertension who is aged over 60 years with the E/e’ >9 can score 5, indicating greater than 80% probability of presence of HFpEF. A slim individual with PAF and hypertension scores 4 points and with other variables and can easily have a greater than 80% probability of HFpEF.
HFA-PEFF
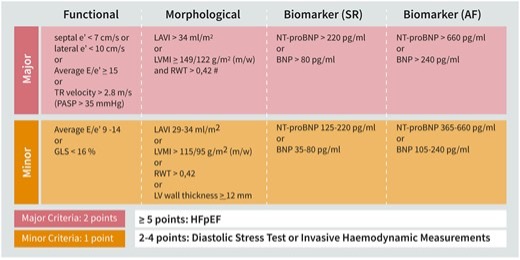
The Heart Failure Association of the European Cardiac Society promotes an alternative algorithm that includes BNP levels and echocardiographic parameters (e’ velocity, E/e’ ratio, left atrial volume and TR jet velocity, as well as others). This algorithm does not include any clinical variables but parameters measured with echocardiography and BNP levels (higher threshold in AF than in sinus rhythm).
An E/e’ ratio >9 has a sensitivity of 78% but specificity of just 59%; an E/e’ ratio > 13 has a lower sensitivity of 46% but higher specificity at 86%. This algorithm assigns two points or one point (major or minor criteria) based on extent of elevation of the included parameters.
Individuals with a score of 2-4 could still have HFpEF but additional testing would be required for confirmation. It is probably true, that in most centres locally, additional testing just to confirm presence of HFpEF is not considered, but can include invasive measurement of pressures or diastolic stress testing with echocardiography.
Pharmacological Treatment
As stated in the European Cardiac Society heart failure guidelines, there is no evidence for benefit if patients are treated with the “standard heart failure drugs” when there is HFpEF, except for SGLT2-inhibitors. Diuretics are indicated to remove congestion.
- Unlike with heart failure with reduced ejection fraction, the European guidelines indicate that only diuretics to relieve congestion and SGLT2-inhibitors are recommended for all patients with HFpEF, other agents indicated as appropriate for co-existent co-morbidties.
- SGLT2-inhibitors reduce the risk of cardiac death and heart failure hospitalisation in those with HFpEF. This benefit is essentially driven by the reduction in heart failure hospitalization and the studies are not powered to show reduction in cardiac death. Some individuals are prepared so self-fund treatment with SLGT2-inhibitors. In the EMPEROR-Preserved trial, over a median of 26 months, the composite of cardiovascular death or hospitalization was 17.1% in the placebo group and 13.8% in the treatment group.
- In the STEP-HFpEF DM trial, patients with obesity related heart failure and type II diabetes treated with semaglutide 2.4mg once weekly had weight loss of around 10% compared to around 3% in the placebo group, with improvement of quality of life, and also improvement in the six-minute walk test. We might speculate that non-diabetic obese patients with HFpEF might also obtain symptom benefit form treatment with a GLP-1 agonist.
- Semaglutide has been studied in obese (BMI 27 or greater) non-diabetic patients with cardiovascular disease, not specifically those with HFpEF. The SELECT trial found that use of the GLP-1 agonist semaglutide 2.4mg weekly had a significant reduction in the primary endpoint of death from cardiovascular cases, non-fatal myocardial infarction or non-fatal stroke, with mean duration of exposure to drug of 34 months, the event rate was 8.0% in the placebo group and 6.5% in the treatment group.
- The TOPCAT study evaluated the potential benefit of treatment with spironolactone in those with HFpEF. The trial was negative, but repeated further analysis over the years has raised the possibility of benefit. When analysis is restricted to patients enrolled in the Americas (hence excluding Georgia and Russia that enrolled, it seems, a different lower risk population group) then there is benefit from use of spironolactone.
- ACE-inhibitors or ARB are first line agents to treat hypertension, spironolactone is also indicated to treat hypertension when additional agents are required, provided renal function is monitored. Many patients with HFpEF have hypertension and arguably we should favour these agents to treat hypertension in this population group.
- Anecdotally, beta-blockers can worsen symptoms in those with HFpEF presumably by excessively blunting the rise in heart rate during exercise. On the other hand, those individuals with resting sinus tachycardia or with excessively fast heart rate response to exercise might obtain symptom benefit from careful titrated prescription of beta-blockers versus the maximum tolerated dose.